Spondyloarthritis (SpA)
Spondyloarthritis (SpA) refers to a heterogeneous family of clinically and genetically related rheumatic diseases characterized by sacroiliitis, spondylitis and peripheral joint involvement (arthritis, enthesitis, dactylitis). In a substantial part of SpA patients, muskuloskeletal involvement is accompanied by extra-articular manifestations (uveitis, psoriasis, and inflammatory bowel disease (IBD)).1
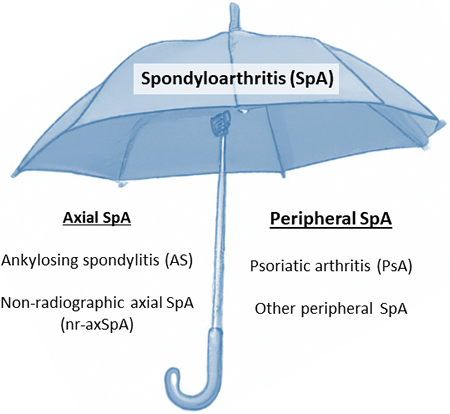
Based on the predominant clinical manifestations in the axial skeleton or the peripheral joints, SpA can be divided into axial SpA and peripheral SpA respectively (See figure below). Axial SpA includes non-radiographic axial spondyloarthritis (nr-axSpA) and ankylosing spondylitis (AS, formerly known as Bechterew’s disease). Peripheral SpA includes psoriatic arthritis (PsA), reactive arthritis, and arthritis associated with IBD.1
Enthesitis and new bone formation are pathognomonic features of SpA.2 It is hypothesized that the threshold for triggering entheseal inflammation is lower in SpA patients. A remarkable tissue response follows the entheseal inflammation, with local new bone formation at the inflamed enthesis as central factor. The appearance of enthesiophytes, new bone formation at the site of the entheses, in patients with psoriasis without apparent articular symptoms highlights the role of enthesitis as early feature in SpA.3
Axial spondyloarthritis (axSpA)
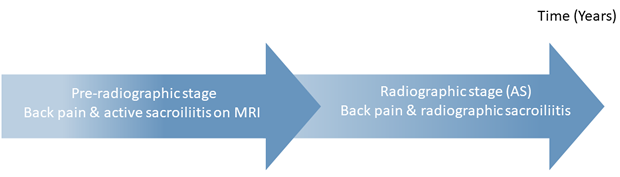
Axial spondyloarthritis (axSpA) is characterized by inflammation of the axial skeleton, i.e. the sacroiliac joints (SIJ) and spine.1 The disease is subdivided into ankylosing spondylitis (AS) and non-radiographic axial SpA (nr-axSpA), based on the presence or absence of radiographic sacroiliitis.4 Advances in the understanding of the progress of the disease led to the consideration of axSpA as a spectrum, with nr-axSpA representing an earlier stage. During this stage, changes detected on plain radiographs might be absent, but inflammation at the SIJ can be detected via MRI.4 (See figure below)
Psoriatic arthritis (PsA)
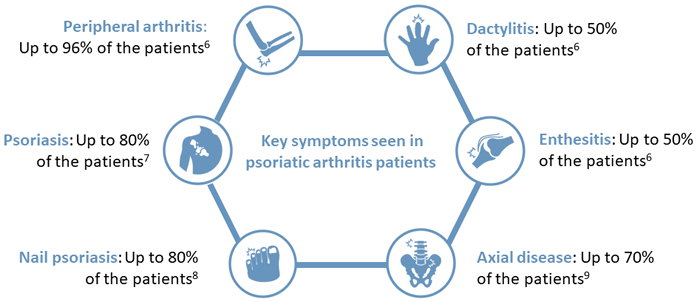
Psoriatic arthritis (PsA) is the most well-studied form of peripheral SpA.1 PsA is characterized by musculoskeletal manifestations accompanied by psoriasis, a chronic inflammatory skin disease.5 About 30% of psoriasis patients have PsA, and skin lesions appear before the musculoskeletal symptoms in the majority of the PsA patients.6,7 Besides psoriasis and peripheral arthritis, ~83% of the patients are affected by nail psoriasis8, up to 50% develop enthesitis and/or dactylitis6 and axial disease is seen in up to 70% of the patients9. (See figure below)
- Garg et al. (2014) Best Pract Res Clin Rheumatol 28, 663-72.
- Schett et al. (2017) Nat Rev Rheumatol 13(12):731-41.
- Simon et al. (2016) Ann Rheum Dis 75, 660–666.
- Rudwaleit et al. (2005) Arthritis Rheum 52(4):1000-8.
- Olivieri et al. (2014) Nat Rev Rheumatol 10(9):531-542
- Ritchlin et al. (2017) N Engl J Med376(10):957-970.
- Gottlieb AB et al. (2006) J Dermatol Treat 17(6):343-352.
- Lee S et al. P&T. 2010;35(12):680-689.
